MADELEINE KLEVEN, SAFE AND HEALTHY FOOD PROGRAM ASSOCIATE, FOOD ANIMAL CONCERNS TRUST
According to new data, the antibiotic resistance crisis is even worse than we thought. A study published in Lancet last week estimates 1.27 million deaths globally were caused by antibiotic resistant-superbugs in 2019. The previous widely accepted estimate from the The Review on Antimicrobial Resistance attributed 700,000 deaths to antibiotic resistant superbugs. While past data has given us a window into this growing global threat, the Lancet article provides a more comprehensive analysis that utilizes additional country specific data as well as deaths associated with a much broader group of antibiotic-resistant superbugs. Though a shocking estimate, it is likely the most accurate representation of the global burden of antimicrobial resistance (AMR) to date.
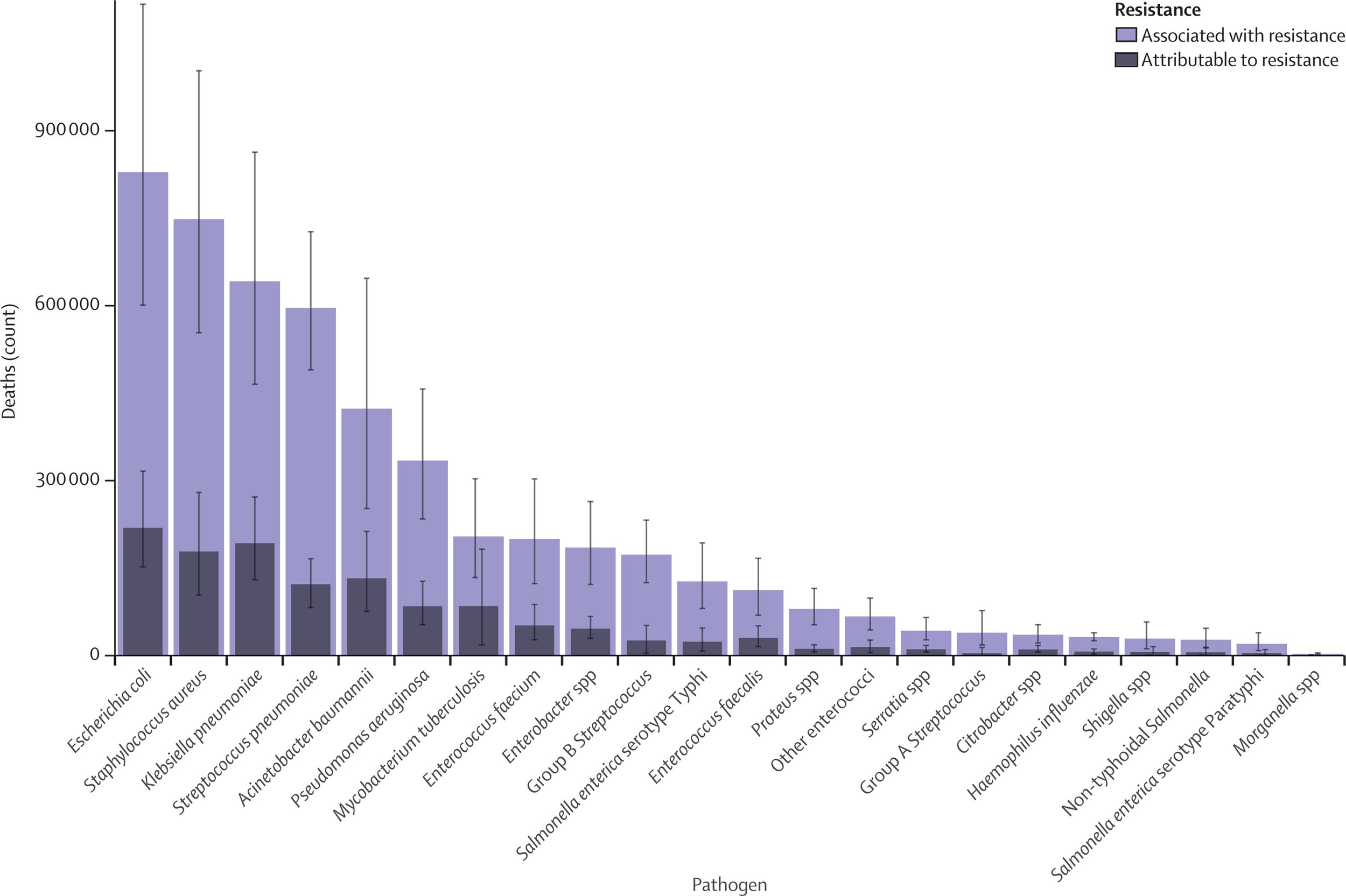
The majority of deaths (approximately 929,000 out of 1.27 million) were caused by six resistant organisms: Escherichia coli, Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa. The remaining 341,000 deaths came from a number of superbugs across several different species. However, these are only deaths directly caused by or attributable to AMR. Many more people died from infections that were resistant, but it was impossible to determine that resistance led to the death itself. In fact, the number of deaths associated with resistant infections was a startling 4.95 million.
This is a true crisis, requiring a rapid and immense response from countries throughout the entire globe.
The emergence of antibiotic resistant superbugs is highly correlated with the overuse of antibiotics both in medicine and in agriculture. In the United States and globally, many more antibiotics are sold for use in food animals than to treat sick people. In the US sales of medically important antibiotics are nearly double the sales for human medicine. Among the top six resistant organisms mentioned above, resistant Escherichia coli and Staphylococcus aureus have been clearly linked to food animals. Resistant Klebsiella pneumoniae and Acinetobacter baumannii are found in food animals and meat. In order to limit the spread of antibiotic resistant organisms in humans, we must limit their spread in animals. Stopping the blatant overuse of antibiotics is key to keeping animals, and in turn humans, healthy.
Improving our nation wide welfare standards for animal production and establishing more strict guidelines for the use of antibiotics is not only a positive suggestion, but an absolute necessity. As the article concludes, “Identifying strategies that can work to reduce the burden of bacterial AMR—is an urgent priority.” Now, more than ever, the U.S. requires leadership to limit the spread of AMR on our own soil and throughout the world.